The off-patent drug that could protect us from future COVID-19 variants
剑桥科学家发现,一种广泛用于治疗肝病的药物可以预防 SARS-CoV-2 感染或减轻新冠重症;
Cambridge scientists have shown that a widely-used drug to treat liver disease can prevent SARS-CoV-2 infection or reduce COVID-19 severity;
该药物副作用小,价格便宜,可能可以预防 SARS-CoV-2 的未来变种;
The drug has minimal side effects, is cheap, and should protect against future variants of SARS-CoV-2;
这项独特的研究涉及“微型器官”、动物研究、捐赠的人体器官、志愿者和患者。
Their unique study involved 'mini-organs', animal research, donated human organs, volunteers and patients.
Scientists have identified a drug that can be repurposed to prevent COVID-19 in research involving a unique mix of ‘mini-organs’, donor organs, animal studies and patients.
这项最近发表在《自然》杂志上的研究表明,用于治疗一种肝病的现有药物能够“锁住”SARS-CoV-2 进入我们细胞的通道,即细胞表面上称为 ACE2 的受体。由于这种药物针对的是宿主细胞而不是病毒,因此它应该可以预防病毒的未来新变种以及可能出现的其他冠状病毒。
The research, published recently in Nature, showed that an existing drug used to treat a type of liver disease is able to ‘lock’ the doorway by which SARS-CoV-2 enters our cells, a receptor on the cell surface known as ACE2. Because this drug targets the host cells and not the virus, it should protect against future new variants of the virus as well as other coronaviruses that might emerge.
如果在更大规模的临床试验中得到证实,它将可能会成为一种重要药物,用于保护那些对疫苗无效或无法获得疫苗的人以及感染风险增加的人。
If confirmed in larger clinical trials, this could provide a vital drug for protecting those individuals for whom vaccines are ineffective or inaccessible as well as individuals at increased risk of infection.
来自剑桥大学Wellcome-MRC剑桥干细胞研究所和阿登布鲁克医院的Fotios Sampaziotis博士与柏林卫生研究所的Ludovic Vallier教授合作领导了这项研究。
Dr Fotios Sampaziotis, from the Wellcome-MRC Cambridge Stem Cell Institute at the University of Cambridge and Addenbrooke’s Hospital, led the research in collaboration with Professor Ludovic Vallier from the Berlin Institute of Health at Charité.
Sampaziotis博士说:“疫苗通过增强免疫系统来保护我们,这样它就可以识别病毒并对其清除,或至少削弱它。但是疫苗并不是对每个人都有效——比如免疫系统较弱的患者——也不是每个人都能接种。此外,病毒可以变异为新的疫苗耐受变种。我们对寻找不依赖于免疫系统、可以补充疫苗接种的替代方法来保护我们免受新冠病毒感染很感兴趣。”
Dr Sampaziotis said: “Vaccines protect us by boosting our immune system so that it can recognise the virus and clear it, or at least weaken it. But vaccines don’t work for everyone – for example patients with a weak immune system – and not everyone have access to them. Also, the virus can mutate to new vaccine-resistant variants. We’re interested in finding alternative ways to protect us from SARS-CoV-2 infection that are not dependent on the immune system and could complement vaccination.”
Sampaziotis 博士之前一直在使用类器官——“微型胆管”——来研究胆管疾病。类器官是可以在培养物中生长和增殖的细胞簇,具有与正在研究的器官部分具有相同功能的3D结构。
Dr Sampaziotis had previously been working with organoids – ‘mini-bile ducts’ – to study diseases of the bile ducts. Organoids are clusters of cells that can grow and proliferate in culture, taking on a 3D structure that has the same functions as the part of the organ being studied.
利用这些,研究人员偶然发现一种被称为FXR的分子大量存在于这些胆管类器官中,它直接调节病毒“通道”ACE2,能够有效地打开和关闭它。通过进一步研究发现,熊去氧胆酸 (UDCA) 是用于治疗一种名为原发性胆汁性胆管炎的肝病的专利到期药物,可“降低”FXR 并关闭 ACE2 通道。
Using these, the researchers found – rather serendipitously – that a molecule known as FXR, which is present in large amounts in these bile duct organoids, directly regulates the viral ‘doorway’ ACE2, effectively opening and closing it. They went on to show that ursodeoxycholic acid (UDCA), an off-patent drug used to treat a form of liver disease known as primary biliary cholangitis, ‘turns down’ FXR and closes the ACE2 doorway.
这项新研究表明,可以使用相同的方法关闭“微型肺”和“微型内脏”(代表SARS-CoV-2的两个主要靶点)中的 ACE2 通道,并防止病毒感染。
In this new study, his team showed that they could use the same approach to close the ACE2 doorway in ‘mini-lungs’ and ‘mini-guts’ – representing the two main targets of SARS-CoV-2 – and prevent viral infection.
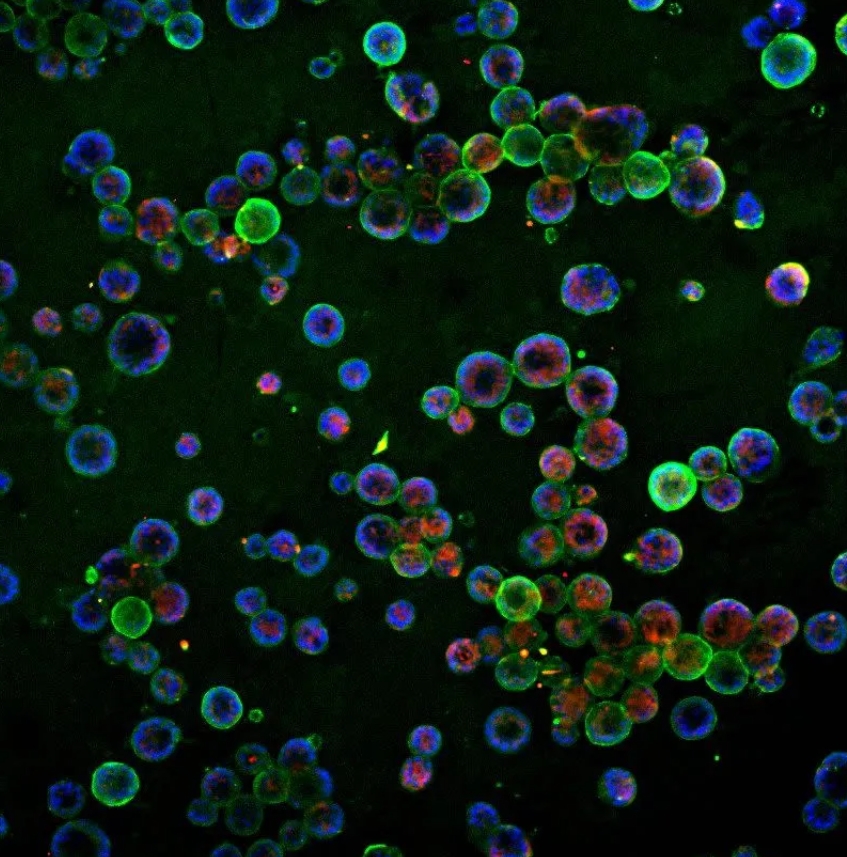
Lung organoids (Credit: Teresa Brevini)
下一步是证明这种药物不仅可以在实验室培养的细胞中预防感染,还可以在活体组织中预防感染。为此,他们与利物浦大学的Andrew Owen教授合作,证明这种药物防止了暴露在病毒下的仓鼠感染,这被用作是抗SARS-CoV-2药物临床前测试的“金标准”模型。重要的是,接受UDCA治疗的仓鼠免受病毒的Delta变体的影响,这种病毒在当时是新型变体,对现有疫苗有部分耐受力。
The next step was to show that the drug could prevent infection not only in lab-grown cells but also in living organisms. For this, they teamed up with Professor Andrew Owen from the University of Liverpool to show that the drug prevented infection in hamsters exposed to the virus, which are used as the ‘gold-standard’ model for pre-clinical testing of drugs against SARS-CoV-2. Importantly, the hamsters treated with UDCA were protected from the delta variant of the virus, which was new at the time and was partially resistant to existing vaccines.
Owen教授说:“尽管我们需要适当的对照随机试验来证实这些发现,但数据提供了令人信服的证据,证明UDCA可以作为一种药物预防新冠,特别是在弱势群体中作为对疫苗的补充。”
“Although we will need properly-controlled randomised trials to confirm these findings, the data provide compelling evidence that UDCA could work as a drug to protect against COVID-19 and complement vaccination programmes, particularly in vulnerable population groups”, said Professor Owen.
接下来,研究人员与纽卡斯尔大学的Andrew Fisher教授和阿登布鲁克医院的Chris Watson教授合作,看看他们在仓鼠身上的发现是否也适用于感染病毒的人类肺部。
Next, the researchers worked with Professor Andrew Fisher from Newcastle University and Professor Chris Watson from Addenbrooke’s hospital to see if their findings in hamsters held true in human lungs exposed to the virus.
研究小组取出了一对捐献的不适合移植的肺,用呼吸机保持它们在体外呼吸,并使用换气设备使血液样液体在它们体内循环,以保持器官功能,同时进行研究。其中一个肺被注射了这种药物,但两个肺都暴露在SARS-CoV-2中。果然,接受药物的那只肺没有感染,而另一只肺却感染了。
The team took a pair of donated lungs not suitable for transplantation, keeping them breathing outside the body with a ventilator and using a pump to circulate blood-like fluid through them to keep the organs functioning while they could be studied. One lung was given the drug, but both were exposed to SARS-CoV-2. Sure enough, the lung that received the drug did not become infected, while the other lung did.
Fisher教授说:“这是首批测试药物灌注时对整个人体器官影响的研究之一。研究结果可能对器官移植很重要——考虑到通过移植器官传播新冠的风险,它可能会开辟在移植前用药物治疗器官以清除病毒的可能性。”
“This is one of the first studies to test the effect of a drug in a whole human organ while it’s being perfused. This could prove important for organ transplantation – given the risks of passing on COVID-19 through transplanted organs, it could open up the possibility of treating organs with drugs to clear the virus before transplantation”, said Professor Fisher.
接下来是人类志愿者,剑桥团队与德国汉堡-埃本多夫大学医学中心的Ansgar Lohse教授合作。
Moving next to human volunteers, the Cambridge team collaborated with Professor Ansgar Lohse from the University Medical Centre Hamburg-Eppendorf in Germany.
Lohse教授解释说:“我们招募了8名健康志愿者接受药物治疗。当我们用棉签擦拭这些志愿者的鼻子时,我们发现ACE2水平较低,这表明病毒很少有机会侵入和感染他们的鼻腔细胞——病毒的主要门户。”
“We recruited eight healthy volunteers to receive the drug. When we swabbed the noses of these volunteers, we found lower levels of ACE2, suggesting that the virus would have fewer opportunities to break into and infect their nasal cells – the main gateway for the virus.”
虽然不可能进行全面的临床试验,但研究人员做了次优选择:查看两组独立患者的新冠病毒数据,将已经因肝脏疾病服用UDCA的患者与未接受该药物的患者进行比较。他们发现,接受UDCA的患者不太可能发展成需要住院治疗的新冠重症。
While it wasn’t possible to run a full-scale clinical trial, the researchers did the next best thing: looking at data on COVID-19 outcomes from two independent cohorts of patients, comparing those individuals who were already taking UDCA for their liver conditions against patients not receiving the drug. They found that patients receiving UDCA were less likely to develop severe COVID-19 and be hospitalised.
论文第一作者、来自剑桥大学的博士生Teresa Brevin说:“这项独特的研究让我们有机会实现真正的转化科学,利用实验室发现直接解决临床需求。我们使用了几乎每一种触手可及的方法,证明了一种现有药物对病毒关闭了大门,可以保护我们免受新冠的伤害。重要的是,由于这种药物是对我们的细胞有效,它不受病毒突变的影响,即使出现新的变异,它也应该有效。”
First author and PhD candidate Teresa Brevini from the University of Cambridge said: “This unique study gave us the opportunity to do really translational science, using a laboratory finding to directly address a clinical need. Using almost every approach at our fingertips we showed that an existing drug shuts the door on the virus and can protect us from COVID-19. Importantly, because this drug works on our cells, it is not affected by mutations in the virus and should be effective even as new variants emerge.”
Sampaziotis博士表示,这种药物可能是一种经济实惠且有效的治疗方式,可以保护那些对疫苗无效或无法获得疫苗的人。“我们已经在临床使用UDCA很多年了,所以我们知道它是安全的,而且耐受性很好,这使得新冠高风险人群可以非常简单地使用它。这种药片成本很低,可以大量生产,快速且容易储存或运输,因此可以在疫情爆发时迅速部署。特别是针对疫苗耐药变种时,它可能是等待新疫苗研发前的唯一防线。我们乐观地认为,这种药物可能成为我们抗击新冠的重要武器。”
Dr Sampaziotis said the drug could be an affordable and effective way of protecting those for whom the COVID-19 vaccine is ineffective or inaccessible. “We have used UDCA in clinic for many years, so we know it’s safe and very well tolerated, which makes administering it to individuals with high COVID-19 risk straightforward. This tablet costs little, can be produced in large quantities fast and easily stored or shipped, which makes it easy to rapidly deploy during outbreaks – especially against vaccine-resistant variants, when it might be the only line of protection while waiting for new vaccines to be developed. We are optimistic that this drug could become an important weapon in our fight against COVID-19.”

 中文
中文 English
English
